Corneal Disease Treatment from The Eye Clinic of Florida
Dr. Mahootchi serves on the medical advisory board of the Lion’s Institute for Transplant and Research. He was the first to perform corneal endothelial transplants in the Tampa Bay area.
Our cornea is the front window of the eye. LASIK changes its shape and the eye’s prescription; dry eyes can make it feel scratchy, and getting something in it sure can hurt. We deal with many cornea problems each day. Learn more about our specialty cornea care center here in Tampa Bay.
The cornea is the clear front surface of the eye. It covers the colored iris and dark pupil. It allows light to pass into the eye and helps to focus the light onto the retina (or the film of the eye). There are many corneal diseases that can affect the clarity and shape of the cornea, which can result in a partial or total loss of vision. When the cornea is cloudy, it is like looking through a dirty window.
Corneal Diseases
There are many reasons why the normal, clear cornea may become cloudy or not focus light correctly on the back of the eye. Viral infections, infections from overwearing contacts, and injuries some of the most common ophthalmic conditions.
Corneal Edema: This is the most common reason to need a cornea transplant. In a healthy eye, the back layer of cells on the cornea (called the endothelium) normally continuously pump water out to keep the cornea tightly packed and to allow light to pass through it undisturbed. With corneal edema (most commonly caused by Fuch’s Dystrophy, these cells do not regenerate and slowly die off during a person’s life. If a person loses too many of these cells, the cornea will swell and become cloudy. Corneal transplants are the most common type of human organ transplants.
Full-thickness corneal transplants are being replaced by endothelial transplants, which just replace the defective part of the cornea. Those transplants go by the names DSAEK, DMEK, and PDEK. The recovery is months faster than the older way of doing it. In fact, recovery in a week is not uncommon.
Tampa has the largest non-profit eye bank in the world so getting tissue is almost never an issue. Insurance, however, is almost always an issue! We can do a transplant, but you need a donor cornea. Think no kidney and the best surgery in the world can’t do a transplant. Some insurances in the Tampa area like to play games with paying for tissue and processing. We can help you navigate the process so you get the best results.

Keratoconus: The normal cornea has a shape like the front portion of a ball. However, some people in young adulthood develop a progressive thinning of the cornea that causes the cornea to develop an irregular shape. This is a slow, progressive disease called keratoconus. As the cornea’s shape becomes more irregular, light rays that enter it are scattered and not focused correctly onto the retina in the back of the eye. Initially, glasses or contact lenses may be able to correct the distortion, and some people with keratoconus may never need surgery. However, other patients’ corneas may become increasingly irregular or scarred to the point that even hard contact lenses will not allow them to see well.
There are cousins of keratoconus like margin pellucid dystrophy and others. These conditions are frequent causes of not being a LASIK candidate. New technology like corneal cross-linking and specialty contacts can help people avoid surgery and see well. Corneal transplants, usually full-thickness transplants, and sometimes a procedure called DALK and Bowman’s Membrane Transplants are surgeries to correct keratoconus. Let Dr. Mahootchi and our team guide you to the best choice for your eyes.
Corneal Scarring: Just like scar tissue can form on a person’s skin; it can also form on the cornea. It most commonly occurs after an infection or trauma. The most common infections that lead to scar tissue are bacterial infections (often after contact lens-related corneal ulcers) or virus infections (such as herpes or zoster viruses). Severe chemical burns may also cause extensive corneal scarring. The right kind of early treatment can make things a lot easier. Early medicine therapy can help avoid surgery. Transplants and other procedures are available for more severe cases.
Corneal Dystrophies: These are abnormalities of specific layers of the cornea that can result in corneal scarring or swelling. Some dystrophies are inherited, but others may develop from new mutations and may not be inherited. Some dystrophies may result in corneal problems in childhood, and others may not manifest until later in life. The most common dystrophy requiring a corneal transplant is Fuchs’ dystrophy, which typically results in corneal swelling that develops later in life.
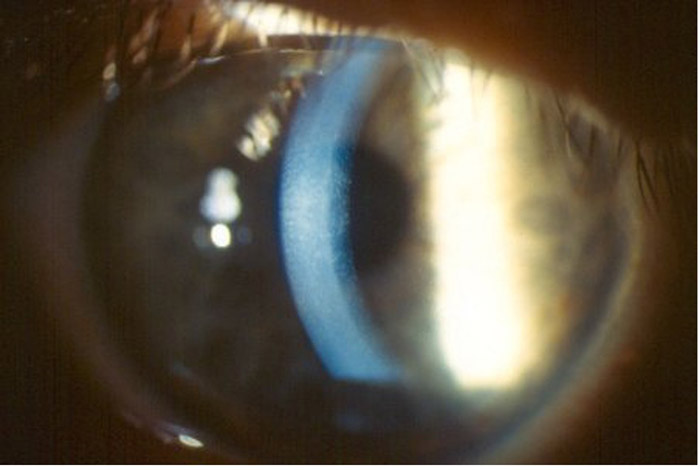 Photo of Fuch’s Corneal Dystrophy
Photo of Fuch’s Corneal DystrophyFailed Corneal Grafts: Some people who have had a cornea transplant in the past may reject the donor tissue, or the tissue may fail by itself after many years. These patients can usually undergo a repeat cornea transplant or sometimes just replace the endothelium as a more simple procedure.
Corneal Transplant FAQ
NOTE: Corneal Transplants and Lens Implants used during cataract surgery are often confused by the general public. Implants are used to replace the cloudy lens during cataract surgery. Corneal Transplants treat a different part of the eye, are less commonly used, and treat diseases and scars of the cornea.
The depends on the type of transplant done. Endothelial transplants ( ultra-thin DSAEK and DMEK) are the most commonly done. These recover in days to a few weeks. The fast recovery and the lower chance of rejection (1% vs 15%) make these a more popular choice.
Full-thickness transplants (called PK or penetrating keratoplasty) take longer to heal and get functional vision. The best vision after a cornea transplant usually requires 4 to 8 months and may continue to improve up to a year after surgery. Most patients will need a different glasses prescription after the surgery to achieve their best vision, and some patients may need to wear hard or soft contact lenses to achieve their best vision. The prognosis for good vision after surgery varies with the disease for which the transplant was performed. The most common indications for a cornea transplant have an 80-90% success rate.
Before surgery:Once you decide to proceed with the surgery, we call the Eye Bank and look for the best tissue available. We usually don’t have a waitlist. We have never had to delay surgery because of donor issues. Before a cornea is released for transplantation, it is inspected for clarity, and the eye bank tests the tissue for different viruses, such as hepatitis and HIV. If you are taking any blood thinners (such as coumadin, Plavix, or aspirin), you may need to stop these medications for a few days before the surgery if it is OK with your primary care doctor. You will be asked not to eat or drink anything for 8 hours before your surgery.
The Day of surgery:The surgery is done on an outpatient basis, which means you will be able to go home on the same afternoon of the surgery. Once you arrive at our Same Day Surgery Center, you will be given some eye drops and a sedative to help you relax. You will also be given some medicine to numb up the eye so that you will not feel any pain.
The operation:Your eyelids will be gently kept open with a lid speculum, so you don’t worry about blinking or keeping your eyes open. The center of the diseased cornea is carefully removed, and any additional work (such as removal of a cataract) is completed. Then the clear, donor cornea is sewn into place. A microscope is used to perform the surgery and the operation takes about 1-2 hours. Drawing that shows steps of a full-thickness corneal transplant. After the diseased cornea is removed-the donor cornea is put into place.
After the operation:A patch and shield will be placed over your eye and you will be allowed to go home after a short stay in the recovery unit. For some, we will ask you to stay on your back as much as you can for the next 2 days
You will need someone to drive you home after the surgery, but once you get home, you will be allowed to eat and perform most activities. You will be able to watch TV and read from your other eye as your operated eye recovers from the surgery. You will come in for a follow-up appointment the day after the surgery. We will ask you to be careful not to rub or get anything in your eye and to use your eye drops as prescribed.
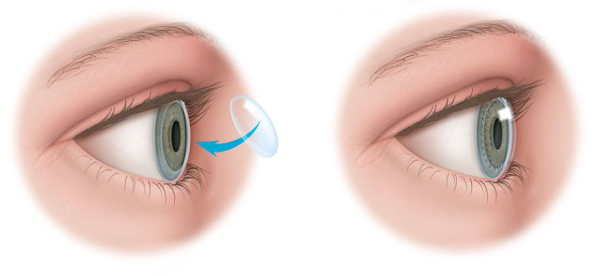
DSAEK (Descemet’s Stripping Automated Endothelial Keratoplasty) and DMEK ( Descemet’s Membrane Endothelial Keratoplasty) are procedures where only the back portion of the central cornea is transplanted, rather than the entire central cornea. This technique may be offered to you if your corneal problem is due to a dysfunction of your corneal endothelial cells (the back layer of the cornea). This procedure is done in a different way from a conventional cornea transplant and requires much less suturing.
Its major advantage is that it typically allows for a more rapid visual recovery and the risk of tissue rejection is also lower with this procedure. About 70% of corneal transplants are done this way throughout the US. However, this procedure can only treat diseases that occur on the back portion of the cornea, so not everyone is a candidate for this procedure. This procedure is also done on an outpatient basis and your experience on the day of surgery will be similar to what has been outlined above for a full corneal transplant.
During the surgery, an air bubble is injected into the front portion of your eye to press the transplanted tissue into position. You will need to lay flat on your back in the recovery unit for one hour after the surgery to allow this process to occur. You will then be allowed to return home, but we will ask you to remain flat on your back as much as possible for the next 1-2 days until the air bubble dissolves away (though you will be permitted to sit up to eat and go to the bathroom). You will still need to be on steroid eye drops for at least a year after the surgery and you will still need to be followed closely after the surgery. DSAEK patients can often experience visual improvement within a few weeks of the surgery and this procedure can also be repeated if necessary. We will let you know if you are a candidate for this exciting new procedure when we examine you.
Please contact us at (813) 538-1503 for an appointment with Dr. Mahootchi or Dr. Huang at The Eye Clinic of Florida or if you have concerns about Corneal Disease and would like more information.
References
- Gorovoy, Mark S. “Sutureless Corneal Endothelial Transplant.” Patient Education Concepts Booklet, 2006. McNeill, James. “Indication and Outcomes of Penetrating Keratoplasty.” Chapter 117, in Cornea, 2004. “Corneal Transplants – A Closer Look.” American Academy of Ophthalmology Patient Education Booklet, 2006 “Corneal Diseases and Surgery.” Wills Eye Hospital Patient Education Booklet, 2006.
Happy Patient Testimonials
Happy Patients Talk About Their Experience with Cataract Surgery and Dr. Mahootchi.